What is cognitive behavioural therapy?
Cognitive Behavioural Therapy (or CBT) is a blend of behaviour therapy, developed by Joseph Wolpe, and cognitive therapy, developed by Aaron T. Beck. Unlike some other therapies, like psychoanalysis, CBT focuses primarily on the present. In other words, instead of focusing on how our past shapes our present concerns, it focuses less on the past and puts a greater emphasis on how current processes are maintaining the problem. In the therapy world, we call this focusing on the here and now.
Research has shown that CBT is effective for treating a variety of mental health problems. It was been shown to be effective in helping individuals with depression, panic, generalized anxiety disorder, phobias (e.g. agoraphobia), obsessive compulsive disorder, (OCD), post-traumatic stress disorder (PTSD), and bulimia (Roth & Fronagy, 2005). It is even effective for helping people with some types of personality disorders.
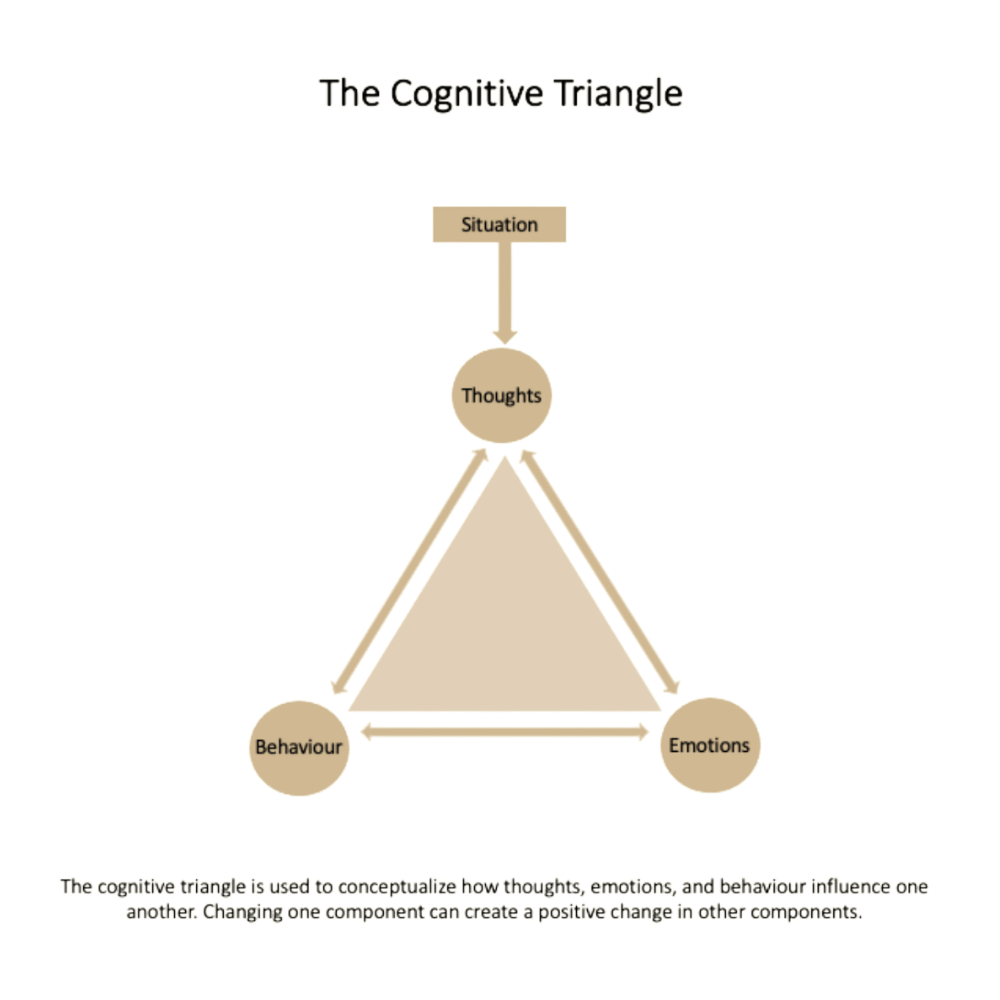
CBT looks at how four main internal systems interact: how we think (cognition), how we feel (emotion), and how we act (behaviour). These systems are thought to be connected because what we do influences our thoughts and emotions. This is a behavioural principle in CBT. Moreover, how we think about events and situations influences our emotions and behaviour. This is the cognitive principle in CBT. CBT combines cognitive and behavioural principles to explain how interactions between thoughts, emotions, and behaviour contribute to the problem.
How CBT changes cognition
CBT therapists work with clients to target three different levels of thought or cognition: automatic thoughts, underlying assumptions, and core beliefs. When starting CBT, therapists will often help the client recognize their automatic thoughts first. Automatic thoughts are quick interpretations that we often don’t recognize unless we pay special attention to them. An example of negative automatic thoughts is, “I’m messing up again”. As you can see, if our brains are riddled with these negative thoughts, it could lead to negative emotions and lead us to act in ways that are unhelpful and prevent us from living a fulfilled and happy life. For example, our negative automatic thoughts can lead us to act defensively, avoid people or situations, or isolate ourselves. CBT therapists help clients identify, reframe, and challenge their automatic thoughts. With practice, the client can learn to recognize and challenge these automatic thoughts themselves, allowing them to become their own therapist and apply CBT skills to daily situations.
CBT therapists also help their clients identify and change fundamental core beliefs about themselves, others, and the world. Like automatic thoughts, core beliefs are usually not immediately identified. It takes effort for us to notice them. Some examples of core beliefs include, “I am unlovable”, “Others can’t be trusted”, and “The world is a dangerous place”. Core beliefs often don’t change much over time or in different situations. They are also often learned early on in our childhood. In comparison to automatic thoughts, core beliefs are more general, more unconscious, and difficult to change.
CBT therapists can also assist clients with identifying and evaluating the underlying assumptions. Underlying assumptions are often unhelpful responses to core beliefs. They often sound like contingencies, meaning they take the form of “if… then” or “should/must… otherwise” statements. An example of an underlying assumption is, “If I always try to please others, they will like me and not abandon me”. They are often found by identifying patterns in behaviours and automatic thoughts.
How CBT changes behaviour
CBT not only targets thoughts, but it targets behaviours too. Behavioural work can take on different forms, depending on the mental health problem being addressed. CBT often targets behaviour through behavioural activation, behavioural experiments, or exposure.
The aim of behavioural activation is to increase helpful behaviours and decrease unhelpful behaviours, thus increasing positive experiences and reducing negative ones. CBT therapists do this by helping clients identify and increase behaviours that provide positive reinforcement. In other words, the therapists help the client identify activities that are enjoyable, increase confidence, and provide connection with others. Behavioural activation also aims to target inactivity and withdrawal from others, which often worsens problems with mood. For example, a client who suffers from depression and tends to ruminate when they are alone might be encouraged to fit more social time into their schedule.
Another way CBT therapists target behaviour is through behavioural experiments. Behavioural experiments are planned experiential activities that challenge clients’ core beliefs and help them create and test more helpful beliefs. While targeting thoughts is helpful, most people learn better from experience, and behavioural experiments allow clients to observe their beliefs through action and observation. For example, a person with social anxiety who believes that everyone is looking at them and judging them when they go out might engage in a behavioural experiment where they look around and count how many people look at them. Such behavioural experiments help clients test out negative beliefs by seeing if the feared outcome actually happens. For example, they might find that only 3 people glanced at them within the 30 minutes that they were in a public place, allowing them to change their belief that others are always looking at them and judging them. Such experiments can be carried out in session, with the support of the therapist, or between sessions, with the client performing the experiment on their own.
A third way that CBT targets behaviours, is through exposure. Behavioural exposure is most often used with clients who avoid feared situations, places, or things. In exposure, the client is exposed to feared stimuli (situations, places, or things), which leads to their anxiety response gradually fading away and the client getting used to the situation and feelings of anxiety. This process of “getting used to” the anxiety and feared stimuli is what is referred to as habituation. Exposure is usually graduated, meaning that the least anxiety-provoking stimuli are tackled first and the most anxiety-provoking stimuli are tackled last. Such graded exposures prevent the client from being flooded or overwhelmed by negative emotions and allows them to confront fear in bite-sized pieces.
Cognitive Behavioural Therapy (CBT) offers a powerful, evidence-based framework for understanding and transforming the patterns of thought and behaviour that contribute to mental health challenges. By addressing both the cognitive and behavioural aspects of psychological distress, CBT empowers individuals to build practical skills that support long-term emotional resilience and well-being. Whether you're struggling with anxiety, depression, OCD, or another concern, CBT provides structured, goal-oriented tools to help you create meaningful change. If you're ready to take the first step toward better mental health, consider speaking with a qualified CBT psychotherapist at Evolve Psychotherapy to explore how this proven approach can support your personal growth and healing journey.
CBT Resources
References
Kennerley, H., Kirk, J., & Westbrook, D. (2016). An Introduction to cognitive behaviour therapy (3rd ed.) SAGE Publications.
Roth, A., & Fonagy, P. (2005). What works for whom: A critical review of psychotherapy research (2nd ed.). Guilford Publications.